What is vaginal prolapse?
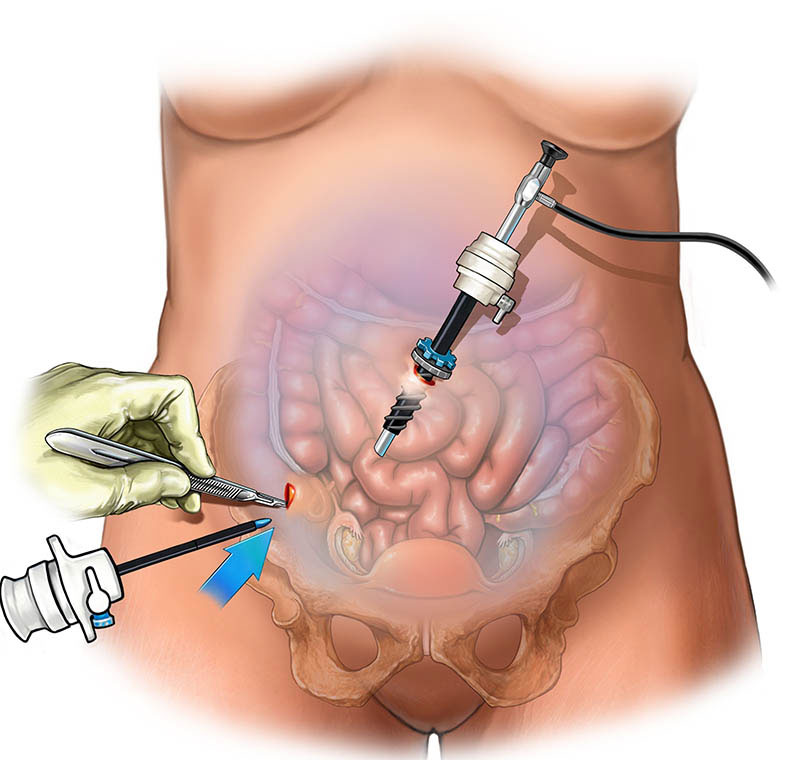
After a hysterectomy, the vagina is held in place by the body’s natural support structures. Vaginal prolapse is a weakening of these support structures that causes the vagina to prolapse into the vaginal entrance where it should be.
The weakening of these support structures depends on whether the uterus has been removed, age, changes in hormone levels, and the number of vaginal births. Vaginal prolapse can affect quality of life. For example, it can cause a feeling of pressure in the pelvic area and discomfort.
What is a laparoscopic sacrocolpopexy?
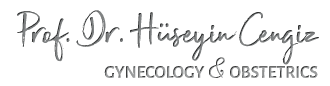
- Laparoscopy: a small needle is inserted into the abdomen through the belly button and the abdomen is filled with gas. The purpose of filling the abdomen with gas is to widen it and make it easier to see the vagina and other pelvic organs. After this procedure, the camera (laparoscopy) is inserted into the abdomen through the belly button. Then two or three smaller incisions are made in the lower abdomen for further surgery.
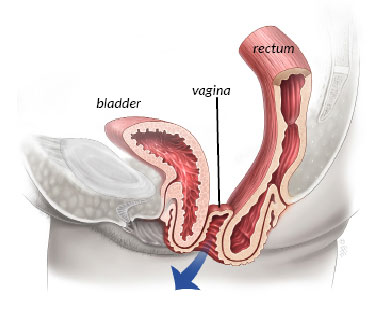
- Sacrocolpopexy: This is an operation in which the vagina is lifted back to its natural position from the back of the vagina to the tail bone (sacrum) with the help of a surgical mesh. The mesh ensures that the vagina remains in its natural position. The picture below shows the mesh adhering to the vagina and sacrum.

Is there an alternative to this surgery?
Mild prolapse can be treated with pelvic floor exercises and vaginal pessaries (usually a plastic ring) without surgery. If you have more severe prolapse symptoms, surgery may be needed. Possible surgeries for vaginal prolapse include vaginal repair with or without mesh, sacrospinous fixation, and sacrocolpopexy (laparoscopic or open). Sacrospinous fixation (a vaginal procedure in which the vagina is attached to the sacrospinous ligament by sutures) and sacrocolpopexy are the most effective surgeries.
What is the success rate of sacrocolpopexy?
Studies have shown that open sacrocolpopexy through the abdomen has a success rate of 74-98.8% and laparoscopic sacrocolpopexy has a success rate of about 92%.
However, because laparoscopic surgery is newer than open surgery through the abdomen, there is less information on how successful laparoscopy is in the long term.
What are the risks during or after surgery?
No surgical procedure is risk-free, and sometimes complications can occur.
The serious risks of laparoscopy include:
- The overall risk of serious complications from diagnostic laparoscopy is about two per 1,000 women (rare).
- Injuries to the bowel, bladder, ureters (tubes through which urine flows from the kidneys to the bladder), or major vessels that require immediate repair by laparoscopy or laparotomy (open surgery) (rare). However, up to 15% of injuries to the bowel may go undetected during laparoscopy.
- Inability to enter the abdominal cavity and inability to perform surgery.
- Hernia formation at the incision site
- Deep vein thrombosis
- Death (3 to 8 per 100,000 women) (very rare)
Common risks associated with laparoscopy include:
- Bruising at the incision site
- Pain in the shoulder
- Opening of the incision site
- Infection at the incision site
Additional procedures that may be required during surgery
- Laparotomy
- Repair of damage to bowel, bladder, ureter, or vessels.
- Blood transfusion
Risks of Sacrocolpopexy
- Postoperative prolapse elsewhere in the vagina requiring surgical correction occurs in 1 to 3 of 10 women.
- Development or worsening of symptoms of urinary incontinence, including stress incontinence or overactive bladder, occurs in about 1 out of 10 women.
- Damage to surrounding organs occurs in 5 out of 100 women.
- Bowel obstruction occurs in 2 out of 100 women.
- In about 5 out of 100 women, the mesh is rejected by the body and the edges of the mesh protrude into the vagina. In this case, the protruding portion of the mesh may be removed; rarely, complete removal is required.
- Infection of the mesh
- Pain during sexual intercourse
- Pelvic infection and abscess formation
Bone infection (rare)
Prevention of blood clotting
Without preventive measures, the risk of developing a blood clot in the leg (deep vein thrombosis) is approximately 15-25% in all patients undergoing surgery. Please discuss the risks of this surgery with your surgeon. You will receive additional information about the measures we have taken to reduce this risk.
What type of anesthesia will be used during surgery?
The surgery will be performed under general anesthesia. You will be asleep and will not feel anything. You will meet the anesthesiologist before surgery and have the opportunity to ask questions about anesthesia.
Prevention of infection
During surgery, you will receive a dose of antibiotics to reduce the risk of infection (prophylactic antibiotics). Additional doses of antibiotics may be given before discharge.
What to expect after the operation?
When you wake up after surgery, you will have a cannula (small plastic tube in a vein) in your hand or arm. You will also have a catheter (drainage tube) in your bladder and a gauze pad (like a large tampon) in your vagina. This is more likely if you had surgery to correct a vaginal prolapse in combination with laparoscopic sacrocolpopexy. If you are wearing a catheter and/or vaginal tampon, the tampon is usually removed the day after surgery. The small incisions in the abdomen will have dissolving sutures and a dressing.
The procedure can be a little uncomfortable, but it is not serious. The nurses will give you pain medicine. Some women may experience bloating and shoulder pain because there is gas under the breathing muscle (diaphragm). This feeling goes away when the gas is absorbed by the body. You will be discharged 24-48 hours after surgery.
Being discharged
If you have undergone vaginal surgery with laparoscopic sacrocolpopexy, you will have some vaginal discharge that may last up to 6 weeks and may vary in color and amount. Sanitary wipes should be used for the discharge instead of tampons. If the discharge turns into bleeding or has a strong, unpleasant odor, you should see your doctor.
The recovery period is usually 3 to 4 weeks. In the beginning, you should avoid strenuous and heavy work and gradually return to your normal life. Swimming is a good exercise after recovery.
Women are at risk of constipation after gynecologic surgery. Be sure to drink plenty of fluids and eat a balanced diet, including fruits and vegetables. You may need to take laxatives because of constipation.
Sexual intercourse may be somewhat uncomfortable at first and should be avoided during the recovery period, as it can interfere with the healing process. It is helpful to use vaginal lubricants initially. After surgery, patients often find that intercourse is more comfortable than before prolapse surgery. Most patients can return to work after 4 to 6 weeks, depending on the type of work.
You should refrain from driving for 2-4 weeks. You can start driving if you do not feel pain during an emergency stop. Practice stopping and backing up in the car before you start driving.
Learning pelvic floor exercises ↓
The pelvic floor muscles are an important support for the vaginal walls, bladder and bowel. They are important for controlling bowel and bladder function.
Lie on your back with your knees bent or sit on a sturdy chair with your knees slightly apart in good posture.
Tighten the ring of muscles around the anus as if you are blocking bowel movements, and then TIGHTEN the muscles around the front ducts, lift them up, HOLD and then slowly release them. Remember to relax your glutes and hamstrings. Breathe normally throughout the exercise.
Exercise program
Try to exercise 3 times a day as described.
- Slow tightening: Tense the pelvic floor muscles and increase the time until you can hold it for a maximum of 10 seconds, aiming for 10 repetitions.
- Fast squeezing: Now quickly squeeze your pelvic floor muscles and then relax them completely. Your goal should be 10 quick squeezes.
- Perform these two exercises while sitting and then begin standing. The goal is for these exercises to become a lifelong habit to support your bladder.
Contact your doctor if any of the following conditions occur after surgery.
- Severe pain
- Fever
- Heavy bleeding
- Foul-smelling discharge
- If one of your legs is painful, hot, red or swollen, this may be a symptom of deep vein thrombosis (blood clot).
- Unexplained shortness of breath, angina, and/or coughing with blood may indicate a pulmonary embolism (blood clot in the lungs).
- Dissatisfaction with the outcome of surgery.
You will be given a follow-up appointment approximately 6-8 weeks after surgery. If you or your doctor feel it is necessary, or if you notice a change or feel uncomfortable, you may contact the outpatient clinic prior to the appointment.